Brain abscess
Intracranial abscesses are rare, potentially lethal intracranial infections. Cerebral abscesses result from pathogens growing within the brain parenchyma, initially as a cerebritis, eventually demarcating into a cerebral abscess.
Intracranial abscesses can originate from infection of contiguous structures (eg, otitis media, dental infection, mastoiditis, sinusitis) secondary to hematogenous spread from a remote site, after skull trauma or surgery, and, rarely, following meningitis. In at least 15% of cases, no source can be identified.
On CT imaging, cerebral abscesses may mimic other space occupying lesions. Clinical presentation may mimic that of brain tumors as well, with sometimes little to no infectious of septic symptoms. MRI can be used to rapidly distinguishing abscesses from tumorous lesions.
MRI features
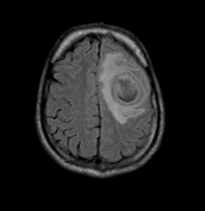
T1: T1 imaging shows a central low intensity (hyperintense to CSF) and often peripheral low intensity due to vasogenic oedema. There is marked ring enhancement and ventriculitis may be present, in which case hydrocephalus may be seen.
T2/FLAIR: Shows central high intensity (hypointense to CSF, does not attenuate on FLAIR) and peripheral high intensity. The abscess capsule may be visible as an intermediate to slightly low signal thin rim.
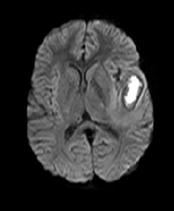
DWI/ADC: The central part of the lesion usually shows a high DWI signal, representing true diffusion restriction with a low signal on ADC. Some peripheral or patchy restricted diffusion may also be seen, although this is not very specific for intracranial abscesses.
SWI: Susceptibility Weighted imaging shows a low-intensity rim that mostly overlaps with the contrast enhancing rim. There may be a dual rim sign, a hyperintense line inside the low-intensity rim.
MR perfusion: rCBV is reduced in the surrounding oedema cf. to both normal white matter and tumour oedema seen in high-grade gliomas.