Radial nerve
The radial nerve is a continuation of the posterior cord of the brachial plexus. It therefore contains fibres from nerve roots C5 – T1.
The nerve arises in the axilla region, where it is situated posteriorly to the axillary artery. It exits the axilla inferiorly (via the triangular interval), and supplies branches to the long and medial heads of the triceps brachii. The radial nerve then descends down the arm, travelling in a shallow depression within the surface of the humerus – known as the radial groove. As it descends, the radial nerve wraps around the humerus laterally, and supplies a branch to the lateral head of the triceps brachii. During much of its course within the upper arm, it is accompanied by the deep branch of the brachial artery.
To enter the forearm, the radial nerve moves anteriorly over the lateral epicondyle of the humerus, through the cubital fossa. The nerve then terminates by dividing into two branches:
- Deep branch (motor) – innervates most of the muscles in the posterior compartment of the forearm.
- Superficial branch (sensory) – contributes to the cutaneous innervation of the hand and fingers.
Click image to enlarge
Motor function
The radial nerve innervates the muscles located in the posterior upper arm and posterior forearm. In the upper arm, it innervates the three heads of the triceps brachii – which acts to extend the arm at the elbow. The radial nerve also gives rise to branches that supply the brachioradialis and extensor carpi radialis longus (muscles of the posterior forearm).
A terminal branch of the radial nerve, the deep branch, innervates the remaining muscles of the posterior forearm. As a generalisation, these muscles act to extend at the wrist and finger joints, and supinate the forearm.
When the deep branch of the radial nerve penetrates the supinator muscle of the forearm, it is termed the posterior interosseous nerve for the remainder of its course
Sensory function
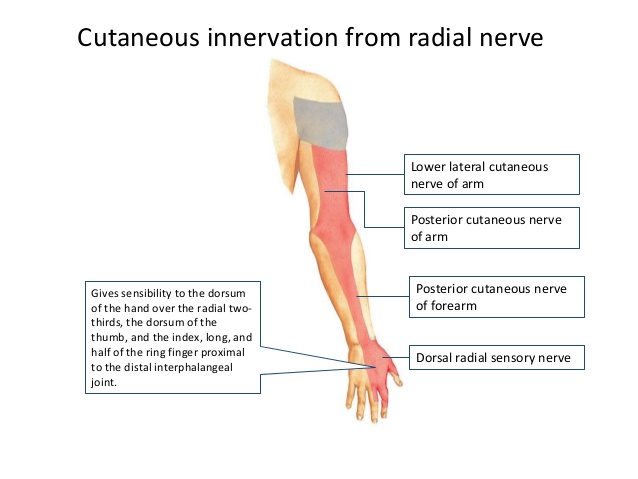
There are four branches of the radial nerve that provide cutaneous innervation to the skin of the upper limb. Three of these branches arise in the upper arm:
- Lower lateral cutaneous nerve of arm – Innervates the lateral aspect of the upper arm, below the deltoid muscle.
- Posterior cutaneous nerve of arm – Innervates the posterior surface of the upper arm.
- Posterior cutaneous nerve of forearm – Innervates a strip of skin down the middle of the posterior forearm.
The fourth branch – the superficial branch – is a terminal division of the radial nerve. It innervates the dorsal surface of the lateral three and half digits, and their associated palm area.
Clinical relevance
Radial nerve palsy in the arm most commonly is caused by fracture of the humerus, especially in the middle third (Holstein-Lewis fracture) or at the junction of the middle and distal thirds. The nerve may be compressed by the lateral intermuscular septum. This palsy may occur acutely at the time of the injury, secondary to fracture manipulation, or from a healing callus.
Other, less common causes of radial nerve palsy in the arm include compression at the fibrous arch of the lateral head of the triceps and compression by an accessory subscapularis-teres-latissimus muscle.
Radial tunnel syndrome
This diagnosis is highly controversial and is thought to be a result of overuse. Some authors believe that radial tunnel syndrome may represent an early posterior
interosseous nerve syndrome. Sites of compression include the fibrous bands attached to the radiocapitellar joint, radial recurrent vessels, the tendinous origin of the extensor carpi radialis
brevis, the tendinous origin of the supinator (ie, arcade of Frohse), and fibrous thickenings within and at the distal margin of the supinator.
Posterior interosseous nerve syndrome
The etiology of posterior interosseous nerve syndrome is similar to that of radial tunnel syndrome. Compression is thought to occur after takeoff of the branches to the radial wrist extensors and the RSN. After emerging from the supinator, the nerve may be compressed before it bifurcates into medial and lateral branches, causing a complete paralysis of the digital extensors and dorsoradial deviation of the wrist secondary to paralysis of the extensor carpi ulnaris.
If compression occurs after the nerve bifurcates, selective paralysis of muscles occurs, depending on which branch is involved. Compression of the medial branch causes paralysis of the extensor carpi ulnaris, extensor digiti quinti, and extensor digitorum communis. Compression of the lateral branch causes paralysis of the abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, and extensor indicis proprius. Most commonly, entrapment occurs at the proximal edge of the supinator.
Other possible etiologies for posterior interosseous nerve dysfunction include trauma (Monteggia fractures), synovitis (rheumatoid), tumors, and iatrogenic injuries.
Wartenberg syndrome, described in 1932, is essentially entrapment of the superficial sensory branch of the radial nerve. Many factors may contribute to the development of Wartenberg syndrome. In patients with de Quervain tenosynovitis, secondary irritation of the RSN is frequent. Other common causes include postoperative injury, external compression, and trauma.
The anatomic site of compression corresponds to the transit of the nerve from its submuscular position beneath the brachioradialis to its subcutaneous position on the extensor carpi radialis longus. Especially with pronation, these two muscles can create a scissorlike effect, compressing the RSN.
Causes of radial nerve dysfunction:
- Improper use of crutches
- Broken upper arm bone
- Long-term or repeated constriction of the wrist (for example, from wearing a tight watch strap)
- Pressure caused by hanging the arm over the back of a chair (for example, falling asleep in that position)
- Pressure to the upper arm from arm positions during sleep or coma
- Pinching of the nerve during deep sleep, such as when a person is intoxicated
- Long-term pressure on the nerve, usually caused by swelling or injury of nearby body structures
- Lead poisoning