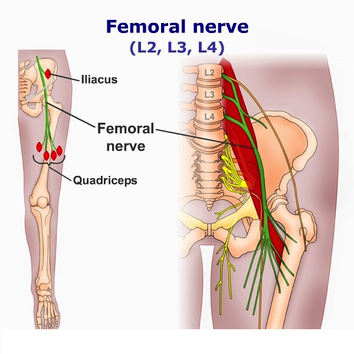
Femoral nerve
The femoral nerve is formed by L2-4 roots and reaches the front of the leg by penetrating the psoas muscle before it exits the pelvis. The femoral nerve leaves the pelvis by passing beneath the medial inguinal ligament to enter the femoral triangle just lateral to the femoral artery and vein. Approximately 4 cm proximal to passing beneath the inguinal ligament, the femoral nerve is covered by a tight fascia, at the iliopsoas groove. The nerve can be compressed anywhere along its course, but it is particularly susceptible within the body of the psoas muscle, at the iliopsoas groove, and at the inguinal ligament.
Motor function
The femoral nerve supplies some of the muscles of the anterior thigh.
Hip Flexors
- Pectineus – adducts and flexes the thigh, assists with medial rotation of the thigh.
- Iliacus – acts with psoas major and psoas minor (forming iliopsoas) to flex the thigh at the hip joint and stabilise the hip joint.
- Sartorius – flexes, abducts and laterally rotates the thigh at the hip joint. Flexes the leg at the knee joint.
Knee Extensors
- Quadriceps femoris (rectus femoris, vastus lateralis, vastus intermedius) – extends the leg at the knee joint. Rectus femoris also steadies the hip joint and assists iliopsoas in flexing the thigh.
Sensory function
The first cutaneous branches of the femoral nerve are the anterior cutaneous branches that arise in the femoral triangle. They supply the skin on the anteromedial thigh.
The last cutaneous branch of the femoral nerve is the saphenous nerve which supplies the skin on the medial side of the leg and the foot.
Click image to enlarge
Clinical relevance
Compression
The femoral nerve is predisposed to compression within the psoas muscle. This commonly is associated with hemorrhage into this muscle due to hemophilia, anticoagulation therapy, or trauma. Direct trauma to the femoral nerve can occur as a result of penetrating wounds or fractures of the hip or pelvis. Intrapelvic masses may also cause compression of the femoral nerve. In addition, compression of the femoral nerve can be due to aortic or iliac aneurysms or tumors.
Lithotomy positioning during delivery or in gynecologic/urologic procedures also has been associated with compressive femoral neuropathy. In this position, the sharp flexion of the hip can compress the nerve at the inguinal ligament. Excessive hip abduction and external rotation cause additional stretch on the nerve.
Diabetes
Patients with diabetes have an unusual predilection for femoral and proximal mononeuropathies. Abnormal femoral nerve conduction has been found in patients with diabetes with no clinical femoral nerve involvement. The etiology is suspected to be an inflammatory vasculitis.
Iatrogenic causes
Iatrogenic causes of femoral mononeuropathy include direct pressure or trauma to the nerve during pelvic, abdominal, or spinal surgery or focal damage at the femoral triangle due to a difficult femoral line placement. Rarely, femoral neuropathy may complicate hip arthroplasty.
Symptoms
Patients with femoral neuropathy complain of difficulty with stairs and frequent falling secondary to "knee buckling." This weakness is typically of acute or subacute onset. On occasion a femoral neuropathy can be associated with an athletic injury. This contrasts with a myopathic process in which the weakness is subacute to chronic in onset and bilateral in nature.
Acute, severe pain in the groin, thigh, and/or lower abdomen may occur if the neuropathy is associated with a retroperitoneal hematoma. Otherwise, the associated pain is usually mild and located near the inguinal ligament.
Patients may complain of medial leg and calf numbness. Sensory symptoms in saphenous nerve distribution are rare with injury to the main trunk of the femoral nerve.
Clinical evaluation
Weakness of the quadriceps muscle and decreased patellar reflex are the most striking examination findings. If the neuropathy is advanced and chronic, wasting of the quadriceps may be noted. If a retroperitoneal hematoma is present, hip extension may cause pain.
In some patients, the iliopsoas muscle is involved. In such cases, the lesion must be above the inguinal ligament, as the motor branch to this muscle comes off before the inguinal ligament.
In isolated femoral neuropathies, the thigh adductors are normal. Although the thigh adductors share common lumbar roots with the muscles innervated by the femoral nerve, they are innervated by the obturator nerve along with the sciatic nerve and therefore are spared. Sensory deficits consist of numbness of the medial thigh and the anteromedial calf.