Strokes and seizures - CADASIL
Case
A 44-year old female visited the emergency department with a generalized tonic-clonic seizure. According to witnesses at the train station, the woman suddenly screamed and fell down on the train platform. Shortly after she developed a seizure. It lasted 3 minutes and was followed by a short postictal phase with confusion and speech impediment. In the ER, the patient complained of headaches. She had a history of migraines, some lasting days, and was currently being treated with venlafaxine (Efexor) for depression and anxiety. She had never had a seizure before, smoked roughly 15 sigarettes per day and denied the use of alcohol. Her father died at age 49, presumably of a stroke. She had a younger sister (41) that suffered from mild cognitive impairment.
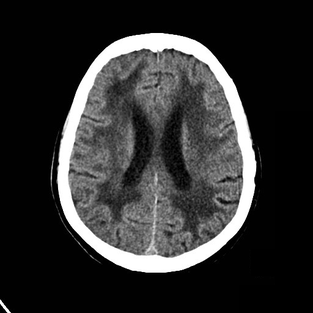
The neurological examination performed in the emergency department showed a mild dysmetria of the left arm and a slightly unsteady gait. An electrocardiogram was made that did not show any pathology. Aside from a slightly high LDL cholesterol (3.9) her laboratory results where unremarkable. A CT scan of the brain was performed:
The CT scan showed extensive white-matter hypodensities and a lacunar infarction in the pons. Consecutively an MRI was made that showed periventricular hyperintensities and characteristic hyperintensities of the external capsule. Our patient was referred to a tertiary neurology center for further examination. Genetic testing revealed a mutation of the NOTCH3 gene on chromosome 19, confirming the diagnosis of cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL).
Background
CADASIL is a rare, inherited vascular brain disease. It typically presents with (repetitive) young onset strokes (often lacunar), migraines with aura, psychiatric disorders, and progressive cognitive impairment. Though seizures have been described in up to 15% of cases, it is very rare for patients with CADASIL to present with a seizure as initial manifestation of disease. With an estimated prevalence of 1-9 per 100.000 adults it is an uncommon disease, though presumably some cases have been misinterpreted as multiple sclerosis, Alzheimer’s disease, or other neurodegenerative diseases before the establishment of genetic testing for CADASIL in 2000.
When CADASIL is suspected based on clinical symptoms and MRI findings, the diagnosis can be confirmed by sural nerve biopsy showing characteristic perivascular deposits of granular electron-dense material resembling immunoglobulin deposits when examined through an electron microscope. Genetic testing reveals a missense mutation in the NOTCH3 gene on chromosome 19. It is thought that mutations in this gene cause NOTCH3 protein segment accumulation in blood vessel walls, leading to accumulation of other proteins and loss of function, scarring the blood vessels, leading to progressive vascular disease.
Summary
Clinical history, including family history, is critical for establishing a diagnosis of CADASIL. Characteristic MRI findings are hyperintense white-matter lesions and repetitive stroke lesions. Think of CADASIL in young patients presenting with recurrent stroke, migrains, and progressive cognitive impairment. Genetic testing and/or sural nerve biopsy confirm the diagnosis.